The ABC’s of CAR T Cell Therapies
 |
All that glitters…
Cancer cells have found ingenious ways to evade the body’s immune system. These cells can shut off cytotoxic activity of anti-tumor T-cells, promoting their own survival. Immunotherapeutic approaches, by design, overcome these tumor mediated inhibitory mechanisms, allowing the patient’s immune system to thwart the invading tumor. Chimeric antigen receptor (CAR) T cell therapies have emerged as the latest immunotherapeutic to show promise against cancers like leukemia (For more information on a CAR T therapy approved for leukemia, check out this blog). But what exactly are CAR T cell therapies?
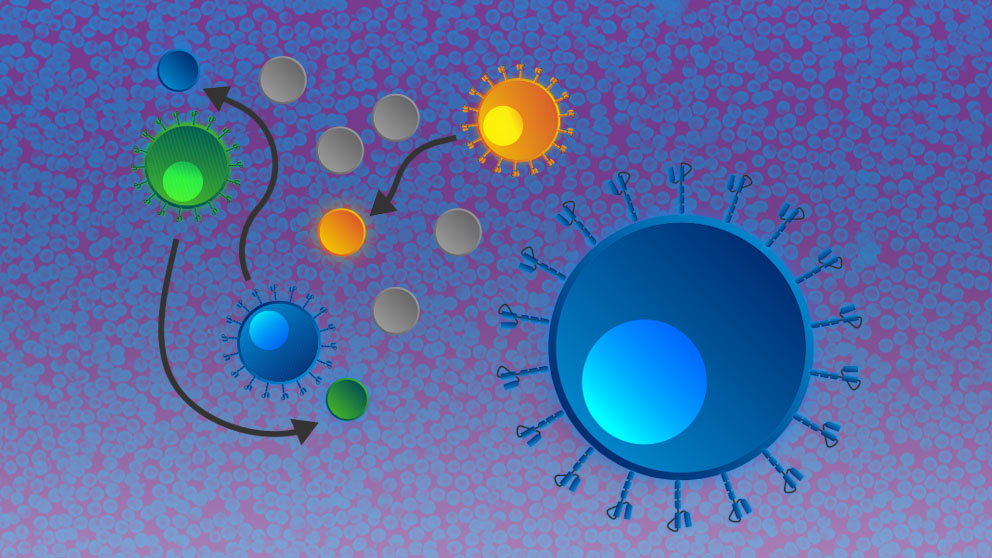
CAR T therapies exploit the antibody-dependent, MHC-independent antigen recognition paradigm by genetically engineering T cells (Daniyan and Bretjens, 2016). First, T cells are removed from a patient, then engineered to express a tumor-specific CAR using gene transfer technology. Finally, the genetically engineered cells are infused back into the patient. The T cells are engineered to express a membrane bound protein that allows the cells to recognize their target antigen on the tumor via single-chain variable fragment (svFV) binding, mimicking way antibodies bind to their target. The svFv portion is linked to an intracellular domain with components that activate the T cell when bound to the target, which results in very effective killing of the cancerous cells (Wang Z et al., 2017; Posey, Jr., et al., 2016). The efficacy of these cells has been observed in CD19+ B cell leukemia’s where cancerous white blood cells circulating within the lymphatic system have a higher likelihood of encountering CAR T cells (Wang et al., 2017).
This therapy offers numerous advantages such as: efficiency of T cell expansion, avoidance of tissue rejection when a patient provides their own T cells, and the possible prevention of tumor recurrence using re-infused CAR T cells.
…Does have parts that are not gold
Although CAR T therapies have shown substantial efficacy in improving outcomes in patients with blood-based malignancies, they do have some limitations. One of the emerging threats, mainly observed in B cell acute lymphoblastic leukemia, is antigen loss relapse, where the expression of the CD19 antigen, in this case, is down regulated in malignant cells. This escape or loss of the antigen is part of the reason why 30-60% of patients relapse after treatment (Xu et al., 2019).
CAR T therapies also requires a high level of personalization of this treatment. As previously mentioned, when patients use their own T cells, the chance of tissue rejection is greatly reduced. However, collecting, expanding, transducing patient cells and then reinfusing them back into the patient increases the difficulty for mass scale production and distribution (Lanitis E. et al., 2020; Wang et al., 2017).
Moreover, with a few exceptions, namely melanoma and renal cell carcinoma, solid tumors are challenging to treat with CAR T cell therapy. Several challenges persist for advancing CAR T cell therapy in solid tumors. First, identifying unique surface markers that distinguish solid tumor cells from healthy tissues has been difficult. As most solid tumor antigens that would otherwise be a target of CAR T therapy are also found on healthy tissues, which presents a risk for toxicity. Secondly, solid tumor antigens are often heterogeneously expressed and can be downregulated, which may result in a therapeutic clonal escape. Ongoing research is focusing on enhancing cellular function as well as reducing the mechanisms of suppression, and despite these limitations, solid tumor studies in mice are bolstering creative problem-solving in the CAR therapy development arena (Lanitis et al., 2020; Day and Daniyan, 2016).
Aside from the limitations of this therapy, there are some additional drawbacks in the form of side effects. CAR Ts, as unique as they are, also present unique toxicities. It’s important to note that the side effects have been observed to be on-target, versus the off-target toxicities associated with chemotherapies. The toxicities occur in the context of tumor cell killing and following either CAR T expansion, eradication, or exhaustion (Santomasso B et al., 2019). The two most notable side effects are cytokine release syndrome (CRS) and neurotoxicity. CRS is defined as the rapid release of proinflammatory cytokines into the bloodstream, and usually presents as a fever or flu-like symptoms in conjunction with hemodynamic instability within the first week of CAR T infusion. Neurotoxity, on the other hand, is characterized with non-pattern specific neurological changes. The severity of these symptoms can vary, depending on many factors, including: disease type and burden, patient age, as well as CAR design and manufacturing conditions, therapy dose, and product potency (Santomasso B et al., 2019; Baymon and Boyer, 2019). However, with continued research and accumulation of data which leads to greater awareness of these toxicities, adjustments are being made to the dosing strategy, resulting in prompt treatment administration and subsequent improvements in prognosis and survival.
Summary
As cancer cells have found ways to avoid the natural immune system, CAR T therapies represent a shining example of combining genetic engineering technologies and immunology. This therapy seeks to harness the power of the immune system, filling in the gaps to help it target and kill cancer cells.
While there are several limitations to the widespread adoption of this therapy due to limitations in mass production and success in specific cancer types, this therapy offers a great deal of hope to patients and is being explored for additional uses. For example, CAR-based strategies in other immune cell types (e.g., CAR-NK) are emerging treatments, and present a viable target for JAX preclinical efficacy studies. Furthermore, the use of comprehensive preclinical studies can enable a better understanding of the interaction in the tumor microenvironment and the engineered cells.