CAR T Cell Therapy, Are We There Yet?
Chimeric Antigen Receptors: licensed to kill
Cancers have cooked up ways to suppress, coerce, and evade the immune system. For instance, cancers can shut off anti-tumor T-cells, thereby promoting their survival. In response, researchers and physicians are exploring immunotherapeutic approaches that are designed to strengthen the immune system’s anti-tumor arsenal. One emerging treatment strategy that is demonstrating considerable promise is Chimeric Antigen Receptor (CAR) T-cell therapy. CAR T-cells are powerful tools that target and destroy cancer cells. The CAR itself is a marriage between an antibody and the signaling portion of a T-cell receptor. T-cells removed from a patient, engineered to express a tumor-specific CAR, and infused back into the patient are now able to effectively kill those cancer cells.
This form of personalized medicine has many advantages:
- T-cells expand well in a lab
- If a patient supplies their own T-cells, tissue rejection is avoided
- Re-infused CAR T-cells may continue to grow and function, preventing tumor recurrence
- The technology to create CAR molecules continues to be improved
Achievements using CARs to mediate regression of leukemias and lymphomas
The U.S. Food and Drug Administration designated immunotherapy as a breakthrough therapy in 2014 based on previous successes and the promise to improve survival outcomes in cancer patients. CAR T-cell therapy currently benefits leukemia and lymphoma patients, with response rates as high as 70-90% in some cases. For this therapy to succeed, CAR T-cells, first, must be able to distinguish diseased cells from healthy cells and, second, must be able to physically interact with their intended target cells. For leukemia and lymphoma, the cell surface marker CD19 distinguishes the tumor cells, allowing the design of a matching, specific CAR. Additionally, CAR T-cells are introduced into the patient’s blood, which allows direct access to both leukemia cells and lymphoid tissues. Together, these key features of blood-based malignancies have made them attractive and effective targets for CAR T-cell therapy.
Improving CAR T-cell therapy
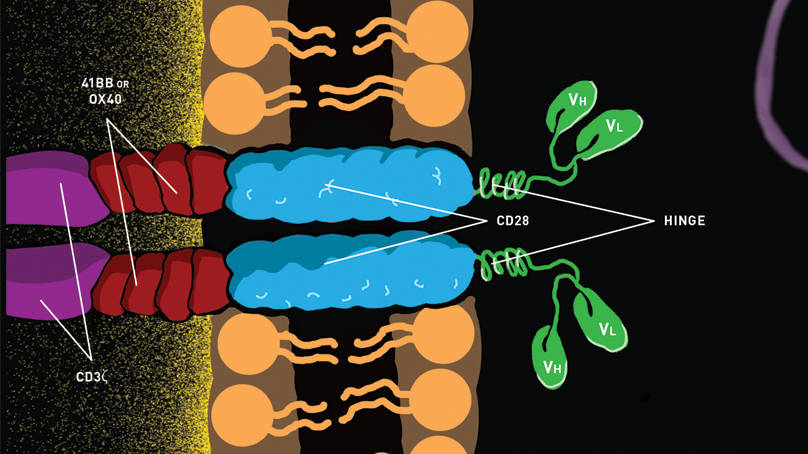
Improvements to CAR T-cell therapy are in development. First generation CAR designs included a simple T cell signaling molecule. Second and third generation CAR designs include T-cell costimulatory domains which lengthen T-cell persistence and tumoricidal activity in mouse models. Use of these newer CAR structures also improves T-cell persistence in patient bloodstreams.
CAR T-cell combination therapies are also being tested. A recent chronic lymphocytic leukemia (CLL) study indicated that adding a novel kinase inhibitor to a CAR T cell therapy improved CAR T-cell expansion in humans and improved tumor clearance and survival in mice. In the clinic, Juno Therapeutics and MedImmune are collaborating to treat non-Hodgkin lymphoma. They plan to use both CAR T-cell therapy and T-cell checkpoint inhibitor blockade, another form of immunotherapy that promotes the immune system’s anti-tumor responses. Combining CAR T-cell therapy with other novel therapies has the potential to dramatically improve patient outcomes by attacking the multiple avenues that a cancer uses to survive.
Toxicity associated with robust CAR T-cell therapy
Although CAR T-cell therapy has strong efficacy in improving outcomes in patients with blood-based malignancies, its successes are not without limits. Two related and significant side effects of using enhanced antitumor T-cells, especially in treating leukemia, are cytokine release syndrome (CRS) and tumor lysis syndrome (TLS). CRS is the quick and massive release of proinflammatory cytokines into the bloodstream; TLS is the quick and massive release of the contents of dying cells into the bloodstream. Together CRS and TLS pose serious health complications. Clinical studies at the National Cancer Institute have indicated that treatment with low dose standard chemotherapy before CAR T-cell therapy reduces toxicity, potentially because the prior, smaller reduction in tumor burden reduces the likelihood of subsequent CRS and TLS.
Limitations to using CAR therapies to treat solid tumors
Based on CAR T cells’ therapeutic success in treating blood malignancies, further refinements to CAR therapeutic approaches are underway that may benefit patients with solid tumors as well. With a few notable exceptions (melanoma and renal cell carcinoma), solid tumors are challenging to treat with CAR T-cell therapy. First, identifying unique surface markers that distinguish solid tumor cells from normal tissues has been difficult. Second, a solid tumor’s structure, the matrix that surrounds it, and its highly immunosuppressive nature, do not permit CAR T-cells to contact their target cells effectively. Despite these limitations, solid tumor studies in mice are bolstering creative problem solving in the CAR therapy development arena.
Future applications for CAR technology in treating solid tumors
Preclinical CAR studies in NSG mice engrafted with patient derived xenografts (PDX) have promising implications for solid tumors. One study identified two markers that are widely expressed in sarcoma cell lines and developed specific CAR T-cells to target them. The CAR T-cells profoundly reduced sarcoma tumor burden and prolonged mouse survival. Another study using patient-derived xenografts of glioblastoma employed CAR technology in a different immune population: natural killer (NK) cells. CAR NK-cells were injected directly into tumors, after which NK-cell anti-tumor activity was observed and the treated animals’ symptom-free survival was significantly increased.
Cancer patients burdened with solid tumors also may benefit from similar, previously described combination strategies. In one study, researchers tested CAR T-cell therapy and T-cell checkpoint inhibitor blockade combinations on sarcomas and mammary tumors in mice. Although CAR T-cells reduced tumor burden and increased mouse survival, including checkpoint inhibitor blockade with the CAR T-cell therapy considerably improved both inhibition of tumor growth and survival outcomes. Successful proof of concept studies in mice such as these pave the way for clinical CAR T-cell therapy for patients with solid tumors.
CAR T-cell therapy certainly has come a long way from its origins in transplant research, where it was learned that T-cells were the responsible parties for graft rejection. Combining an antibody’s ability to specifically recognize a tumor with a T-cell’s power to eliminate it culminates in a clever technology that is sure to drive further innovations in cancer treatment.